That would be cool. Getting treated based on needs that addresses the missing component. I'll be positive and not bitch about the fact that they aren't looking to zoom up on what the cause is that is changing the cells in the first place. Something is causing them to respond to certain factors a certain way. That's a post for another day. This study was positive though. Maybe this can lead to treatments that can improve the quality of life in people that suffer from IBD/gastrointestinal disturbances. We can only hope that treatments will be better and safer. So, Washington University researchers used biopsy cells, taken from patients during a routine endoscopy to study if epithelial cells could be grown in the lab if therapeutic conditions were provided. According to the article, cells were obtained and placed in "a high concentration of conditioned media containing the factors critical for growth (Wnt3a, R-spondin and Noggin)". Within 2 weeks, the result from these conditions were positive. They showed that epithelial cells formed "functional, polarised monolayers covered by a secreted mucus layer when grown on Transwell membranes". They also exposed the cells to bacteria (e. coli) to see how they would respond when exposed to harmful bacteria changes. The results were favorable.
Technology for the growth of human intestinal epithelial cells could help scientists develop individualized therapies for inflammatory bowel disease and other gastrointestinal conditions. This is the conclusion of a group of researchers at Washington University School of Medicine in St. Louis, who recently published a study, entitled, “Development of an enhanced human gastrointestinal epithelial culture system to facilitate patient-based assays,” in the Journal Gut.
For this to be possible, the team explained in the abstract of their study that epithelial cells must be enhanced so that biopsies from patients can be used to generate cell lines (which are populations of cells in culture with the same genetic makeup) in a short time frame, so that the analysis can be made accurately.
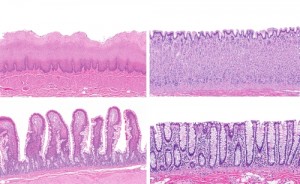
In two weeks, researchers were able to create 65 human gastrointestinal epithelial cell lines from biopsies of 47 patients, taken during routine endoscopic screening procedures. They used a high concentration of conditioned media containing the factors critical for growth, which resulted in a rapid expansion of the proliferative stem and progenitor cells. In addition, the team used a combination of lower conditioned media concentration and Notch inhibition to differentiate these cells for further research.
Results showed that under differentiation conditions, intestinal epithelial spheroids developed mature epithelial lineages in specific regions. These cells formed functional, polarized monolayers covered by a secreted mucus layer when grown on Transwell membranes.
After this process, researchers conducted experiments to determine how the cells interacted with bacterial pathogens like Escherichia coli. They found the cells also demonstrated novel adherence phenotypes with various strains of pathogenic Escherichia coli.
Ultimately, these findings can help testing of new drug targets, as well as developing vaccines. Furthermore, they will play a crucial role in understanding how human cells interact with beneficial and harmful microbes, researchers believe.
Link to the abstract journal article in Gut - http://gut.bmj.com/content/early/2014/07/09/gutjnl-2013-306651.abstract?sid=79c1ef19-7ade-4f0b-99cf-aadfe542fd76
No comments:
Post a Comment