My naturopathic doctor is great! I'm passing on what she has recommended to me to whomever it can help.
If you have a vitamin/mineral deficiency, you could go years not feeling well and struggling. Your regular PCP/MD just don't do a thorough enough test to determine all your needs. Doctors are on the vitamin D train now... hopefully, but what else might your body be lacking?
BodyBio is a blood test that will determine vitamin levels/needs. Check it out if you think you are deficient OR if you have a disease like Crohn's colitis. Inflammation in the digestive system will hinder the absorption of the nutrients from your foods and supplements. Most people with a digestive disease probably have malabsorption issues and nutrient deficiencies.
Just from the top of my head, B vitamins, iron, D, mag, calcium, zinc, C, iodine, K
Here's the link to the main page for the test - BioCell|Home:
If you have a vitamin/mineral deficiency, you could go years not feeling well and struggling. Your regular PCP/MD just don't do a thorough enough test to determine all your needs. Doctors are on the vitamin D train now... hopefully, but what else might your body be lacking?
BodyBio is a blood test that will determine vitamin levels/needs. Check it out if you think you are deficient OR if you have a disease like Crohn's colitis. Inflammation in the digestive system will hinder the absorption of the nutrients from your foods and supplements. Most people with a digestive disease probably have malabsorption issues and nutrient deficiencies.
Just from the top of my head, B vitamins, iron, D, mag, calcium, zinc, C, iodine, K
Here's the link to the main page for the test - BioCell|Home:
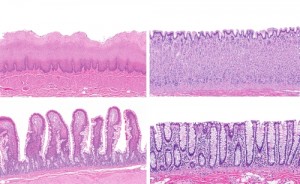
This is a screenshot of one of the example diagnostic pages .